Let’s be honest: menstrual pain is no joke. I still remember my first period—I was curled up on the couch with a hot water bottle, wondering if this was what everyone else went through. Turns out, many women experience similar discomfort every month. For many women, intense pain from period cramps can be a monthly challenge that interrupts daily life. The good news? There are plenty of ways to ease the discomfort and take control of your menstrual health. In this post, we’ll explore why period pain happens and how you can reduce it with remedies, treatments, and simple lifestyle changes.

Caption: A comforting moment of self-care with a hot water bottle and tea during menstrual discomfort.
Understanding Menstrual Pain
Your menstrual cycle is a natural process where the uterus sheds its lining, similar to how trees shed their leaves in autumn to prepare for new growth. This biological reset allows your body to maintain a healthy reproductive system. This involves contractions of the uterine muscle, which can cause cramping pain, especially in the lower abdomen. Primary dysmenorrhea refers to the common period cramps many women experience, while secondary dysmenorrhea indicates an underlying condition, such as pelvic inflammatory disease or ovarian cysts. According to the Mayo Clinic, understanding the difference between primary and secondary dysmenorrhea is crucial for effective treatment.
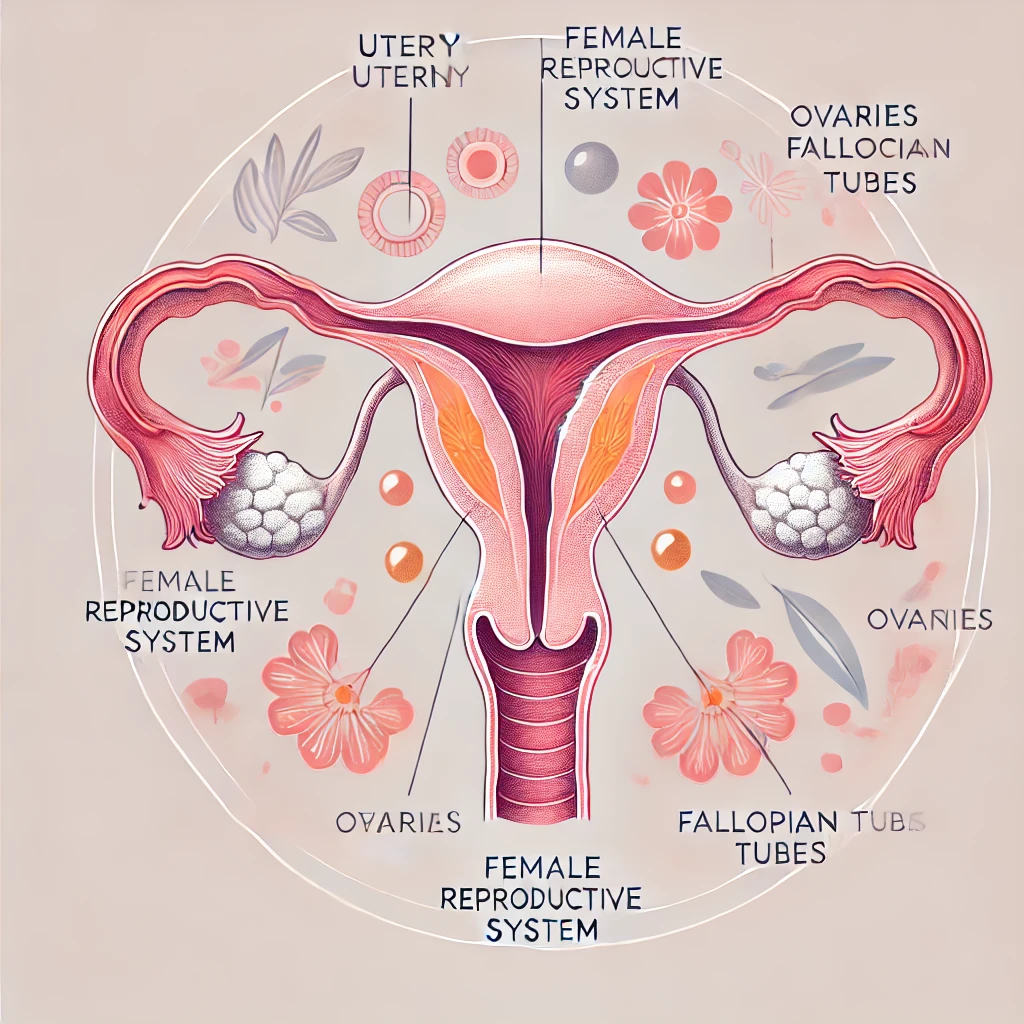
Caption: An artistic and educational illustration of the female reproductive system, highlighting key organs with soft, feminine tones.
Common Causes of Period Pain
Period pain, also called dysmenorrhea, occurs because of:
- Uterine muscle contractions: These tighten blood vessels and cause pain.
- Secondary conditions: Issues like non-cancerous growths, infections, or cervical stenosis can lead to painful periods.
- Reproductive health factors: Irregular menstrual bleeding, abnormal vaginal fluid, or infections caused by sexually transmitted bacteria may worsen symptoms.
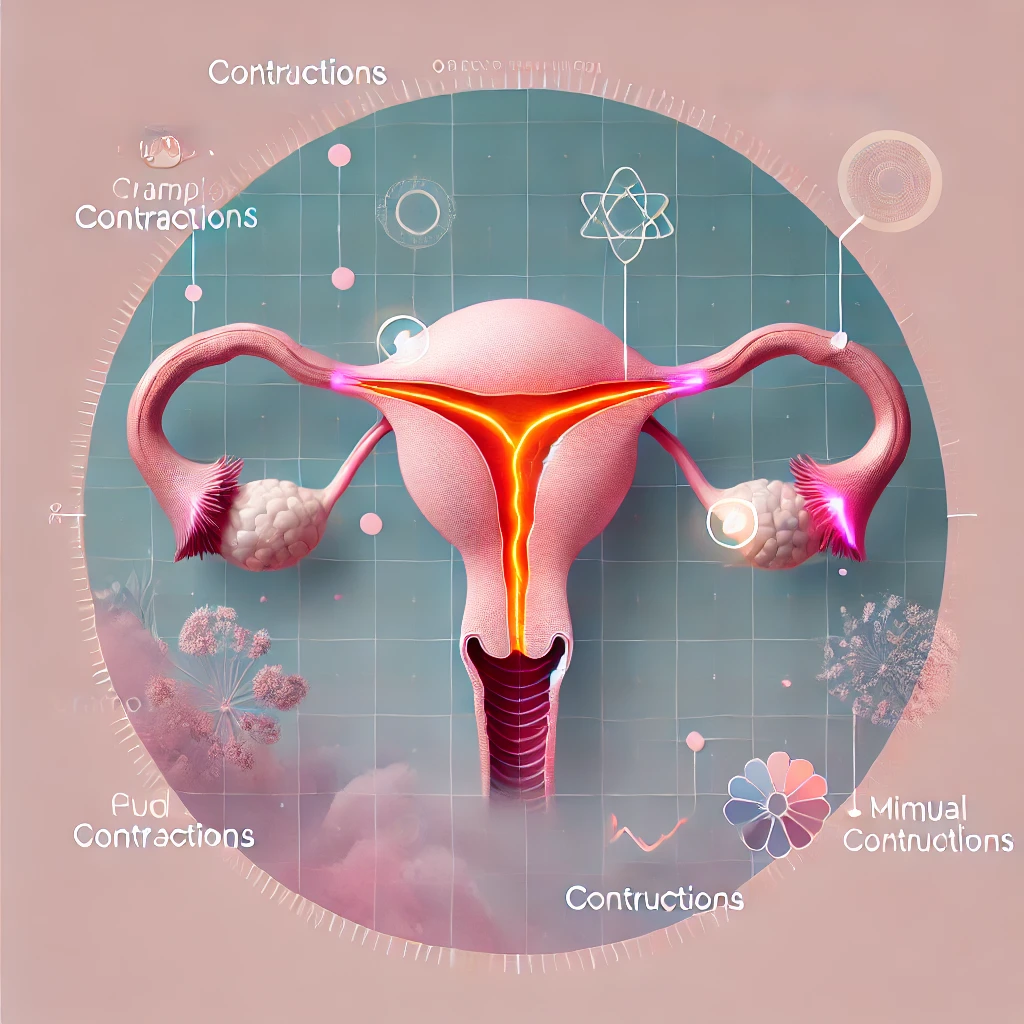
Caption: A conceptual illustration of the uterus highlighting areas affected by cramps or contractions, in soothing feminine tones.
Recognizing Symptoms
Period pain varies from mild cramping to intense discomfort. You might feel:
- Cramping pain in your lower abdomen.
- Severe pain radiating to your back or thighs.
- Other symptoms like irregular bleeding or pelvic cramping.

Caption: A thoughtful woman reviewing her calendar, symbolizing the importance of tracking menstrual cycles and symptoms.
Diagnosing the Cause of Menstrual Pain
Simple Remedies to Reduce Menstrual Pain
- Home Remedies:
- Use a heating pad or hot water bottle on your lower abdomen.
- Take a warm bath to relax uterine muscles.
- Apply gentle pressure with your hands.
- Consider taking an over-the-counter pain reliever like ibuprofen to alleviate menstrual cramps.

Caption: A flat lay of soothing self-care items, including a heating pad, essential oils, and herbal teas, perfect for relaxing during menstrual pain.
- Stay Active:Light physical activity, such as yoga or walking, can improve circulation and ease cramping. Specific yoga poses like Child’s Pose, Cat-Cow Stretch, and Reclining Twist are particularly effective for targeting the lower abdomen and relieving tension.

Caption: A serene scene of a woman practicing yoga, performing Child’s Pose to ease menstrual discomfort and promote relaxation.
- Dietary Tweaks:Reduce inflammatory foods and drink plenty of water. Maintaining a healthy weight may also reduce symptoms.
- Alternative Therapies:Consider acupuncture, which stimulates specific points on the body to promote relaxation and improve blood flow, potentially reducing menstrual pain. Other alternative therapies, like aromatherapy with essential oils or reflexology, have also shown promise for easing discomfort.
Medical Treatments for Severe Period Pain
Sometimes, remedies aren’t enough. Here are medical options:
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen work wonders.
- Hormonal birth control: These regulate your cycle and reduce intense cramping.
- Treating underlying conditions: If pain stems from infections or noncancerous growths, targeted treatments may be necessary.

Caption: A professional healthcare provider offering reassurance and guidance to a patient in a warm, inviting clinic environment.
eLifestyle Changes to Manage Menstrual Cramps
Adopting certain lifestyle changes can significantly reduce the severity of menstrual cramps and make your periods more manageable. Here are some effective strategies:
- Exercise Regularly: Physical activity releases endorphins, which are natural pain relievers. Aim for regular exercise to help reduce menstrual cramps.
- Maintain a Healthy Weight: Being overweight or obese can exacerbate menstrual cramps, so maintaining a healthy weight is beneficial.
- Reduce Stress: Stress can worsen menstrual cramps. Techniques like meditation, yoga, and deep-breathing exercises can help manage stress levels.
- Get Enough Sleep: Adequate sleep helps regulate hormones and reduce stress, both of which can lessen menstrual cramps.
- Eat a Healthy Diet: A diet rich in fruits, vegetables, and whole grains can reduce inflammation and promote hormone balance, helping to reduce menstrual cramps.
- Avoid Triggers: Identify and avoid foods and beverages that can worsen menstrual cramps, such as caffeine, alcohol, and certain processed foods.
By incorporating these lifestyle changes, you can experience less menstrual pain and improve your overall well-being.
Prevention Tips
You can proactively reduce menstrual cramps with these tips:
- Exercise regularly to improve circulation.
- Avoid untreated infections by practicing safe habits.
- Manage stress and maintain hormonal balance through a healthy lifestyle.

Caption: A vibrant scene of a woman jogging in a park, radiating health and positivity, symbolizing an active lifestyle for better menstrual health.
Menstrual Cramps and Other Health Conditions
Menstrual cramps can sometimes be a symptom of other underlying health conditions. It’s important to be aware of these conditions and seek medical advice if you experience severe or persistent cramps:
- Pelvic Inflammatory Disease (PID): This bacterial infection causes inflammation and scarring in the reproductive organs, leading to painful menstrual cramps.
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and severe cramps.
- Uterine Fibroids: Non-cancerous growths in the uterus that can cause significant menstrual pain.
- Adenomyosis: A condition where tissue similar to the uterine lining grows into the uterine muscle, leading to inflammation and severe cramps.
- Hormonal Imbalances: Conditions like polycystic ovary syndrome (PCOS) can cause hormonal imbalances that result in painful menstrual cramps.
If you experience severe or persistent menstrual cramps, it’s essential to consult your healthcare provider. They can help diagnose any underlying conditions and recommend appropriate treatments to manage your symptoms effectively.
FAQs About Menstrual Pain
1. What does period cramping feel like?
It’s a cramping or aching pain in the lower abdomen, sometimes spreading to the back or thighs.
2. Is severe period pain normal?
Mild pain is common, but severe pain may indicate an underlying condition. Seek medical advice if it’s debilitating.
3. How can I quickly ease menstrual cramps?
Try a heating pad, take NSAIDs, or relax in a warm bath.
Additional Resources
For more information, check out these helpful links:
- American College of Obstetricians and Gynecologists
- Mayo Clinic’s Guide to Dysmenorrhea
- Planned Parenthood’s Reproductive Health Resources
Conclusion
Managing menstrual pain doesn’t have to feel impossible. With the right strategies and support, you can turn a difficult experience into a manageable one, empowering yourself to live life on your own terms. Whether you’re trying home remedies, adjusting your diet, or consulting a doctor for severe symptoms, there are solutions that work for you. Take control of your menstrual health and embrace a pain-free cycle.
All the helpful resources mentioned above can be found at:
American College of Obstetricians and Gynecologists, Mayo Clinic’s Guide to Dysmenorrhea, and Planned Parenthood’s Reproductive Health Resources.