Vulvovaginitis is inflammation of the vulva and vagina, causing itching, discharge, and irritation. This article explains its causes, symptoms, and treatments.
Key Takeaways
- The primary causes of vulvovaginitis include bacterial vaginosis, yeast infections, and sexually transmitted infections, leading to various symptoms such as abnormal discharge and genital discomfort.
- Diagnosis involves a comprehensive examination and laboratory testing to identify the specific cause of vulvovaginitis, which is crucial for effective treatment.
- Treatment varies based on the underlying cause, requiring targeted therapies such as antifungals for yeast infections and antibiotics for bacterial vaginosis, complemented by preventative measures and lifestyle adjustments.
Common Causes of Vulvovaginitis

Vulvovaginitis is commonly induced by bacterial vaginosis, a condition stemming from an imbalance of natural bacteria within the vagina. This often results in unusual vaginal discharge that may appear grayish-white and exude a potent fishy odor.
Fungal overgrowth, specifically Candida albicans, constitutes the second most prevalent cause for vulvovaginitis leading to yeast infections. These are characterized by genital itching and a thick white discharge with an appearance similar to cottage cheese.
Sexually transmitted infections (STIs) including trichomonas, chlamydia, gonorrhea, and herpes simplex virus can give rise to vulvovaginitis as well. Typically associated with symptoms like burning sensations during urination or intercourse along with abnormal discharges—these conditions might contribute to genitourinary syndrome’s signs and other indicators such as inflammation in the genital area. It’s noteworthy that STIs might not always manifest outwardly noticeable symptoms.
A clear understanding of these typical factors causing vulvovaginitis lays the groundwork for effective identification and management of this issue, which is crucial for maintaining optimal vaginal health and comfort levels.
Bacterial Vaginosis
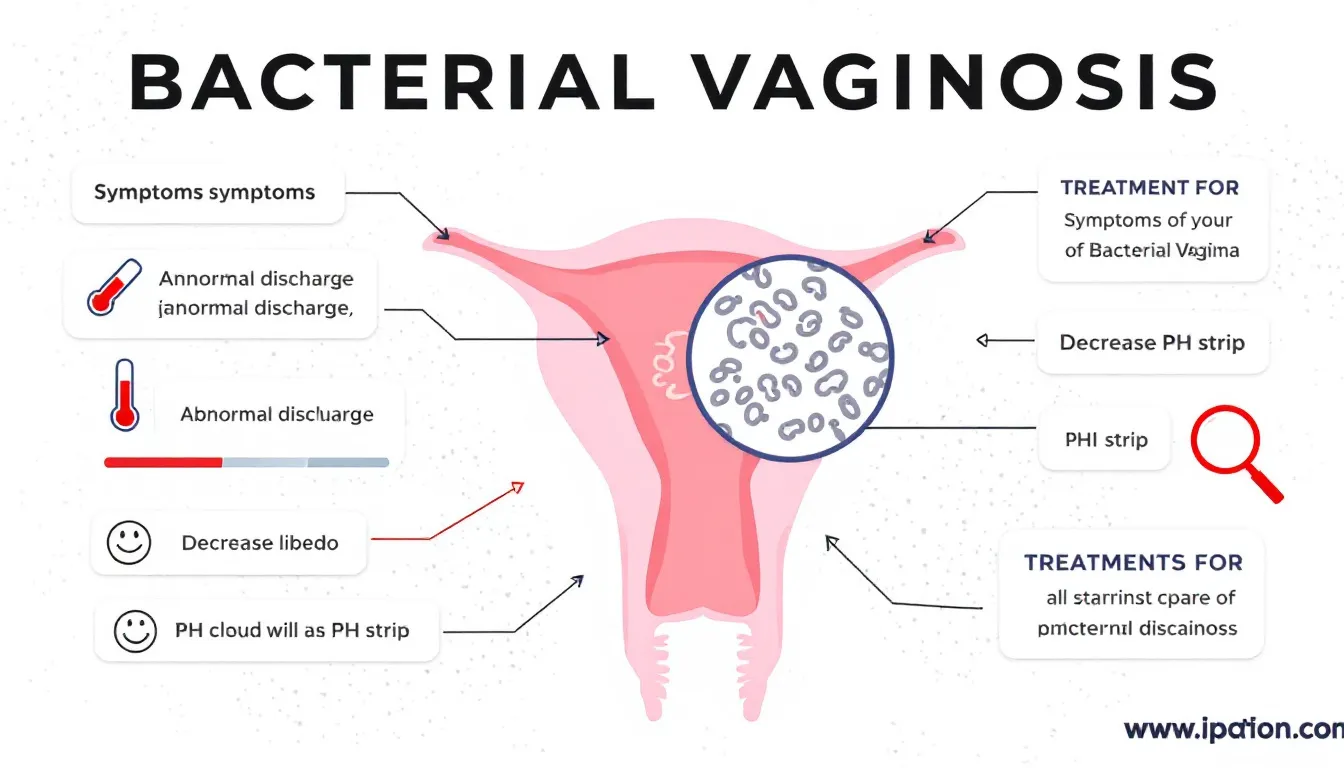
Bacterial vaginosis is recognized as the most common type of vulvovaginitis, resulting from a disturbance in the vaginal flora. Ordinarily, Lactobacillus species colonize the vagina and play a crucial role in preserving its healthful state. A decline in these beneficial bacteria can give rise to an overgrowth of pathogenic microorganisms like Gardnerella vaginalis, often causing recurrent episodes of bacterial vaginosis. This disorder typically manifests with symptoms such as grayish-white discharge emitting a potent fishy odor – this distinctive sign sets it apart from other types of vaginal infections.
The dominance of pathogens like Gardnerella vaginalis overrides the customary bacterial ecosystem within the vagina, which creates this disequilibrium. Although additional bacteria including Streptococcus and Staphylococcus might also be found here, they usually aren’t implicated as causative agents during incidents of bacterial vaginosis.
It’s critical for effective treatment and management to recognize signs promptly and comprehend that asymptomatic bacterial vaginosis stems from an underlying imbalance among different bacteria inhabiting the vagina.
Yeast Infections
Vulvovaginitis caused by Candida species, particularly the prevalent fungus Candida albicans, is a frequent type of vaginal infection. This organism proliferates when there’s an imbalance within the vaginal flora, leading to symptoms that predominantly consist of severe genital and vaginal itching. Accompanying these symptoms are discharges similar in appearance to cottage cheese. If not adequately treated, such infections can persistently recur, causing discomfort through both general yeast infections and more specifically diagnosed as a vaginal yeast infection.
Antibiotic usage often initiates yeast infections due to its tendency to disrupt the equilibrium of healthy bacteria within the vagina – conditions under which candida multiplies freely. It’s crucial for maintaining balanced vaginal health and utilizing antibiotics judiciously in order to prevent this overgrowth.
Being aware of what triggers yeast infections along with recognizing their signs is essential for procuring prompt treatment and averting repeated episodes associated with these fungal concerns.
Sexually Transmitted Infections (STIs)

Vulvovaginitis can often be attributed to sexually transmitted infections, with Trichomonas vaginitis, Chlamydia, gonorrhea, and herpes being the primary pathogens involved. Trichomonas vaginitis typically presents with a range of unpleasant symptoms such as genital discomfort and itching. It is characterized by an odorous heavy discharge that may appear yellow-green and frothy in nature—complications which contribute to various vaginal complaints.
To mitigate the risk of contracting STIs capable of causing vulvovaginitis, engaging in protected sexual practices like using condoms is highly advised. It’s also crucial for individuals to communicate potential exposures to their sexual partners promptly so as to manage existing cases effectively while preventing subsequent reinfections. Such strategies aimed at notifying partners enable treatment before they exhibit clinical signs themselves—which cuts down on Spread—thereby fostering improved overall sexual health within populations.
Non-Infectious Causes
In some instances, vulvovaginitis is not triggered by infectious agents but rather through non-infectious means. External irritants such as abrasive soaps, feminine hygiene products like sprays, or restrictive clothing can lead to the condition. The continuous exposure to these elements may result in enhanced inflammation and discomfort within the vaginal region. Environmental allergens have the potential to aggravate symptoms. Identifying and steering clear of these catalysts is essential.
Another factor contributing to non-infectious vulvovaginitis is vaginal dryness, which is frequently associated with hormonal shifts or conditions such as atrophic vaginitis. Persistent irritation from these sources can impede recovery processes and intensify the severity of vulvovaginitis by compromising the integrity of the vaginal epithelium.
Grasping an understanding of what contributes to noninfectious causes behind vulvovaginitis proves indispensable for effective prevention and control measures that are aimed towards fostering optimal vaginal well-being.
Diagnosing Vulvovaginitis

The process of diagnosing vulvovaginitis is thorough, beginning with a physical exam to look for indications such as redness around the vulva and abnormal vaginal discharge. When suspecting vaginitis, laboratory assessments like testing vaginal pH levels, conducting a potassium hydroxide (KOH) whiff test, and utilizing wet mount microscopy are typically performed. These procedures are crucial in determining if bacterial, fungal or parasitic infections are at the root of the condition.
Taking an in-depth look into patient history and medical records is essential during diagnosis since it provides insight into past occurrences, personal hygiene habits, and potential allergens that might trigger an allergic reaction. Should symptoms continue despite initial treatments being administered—a biopsy might be suggested to exclude other diseases or verify the suspected diagnosis—accurate identification of what’s causing the illness is vital for effective treatment plans tailored towards resolving vulvovaginitis.
Treatment Options for Vulvovaginitis

The approach to managing vulvovaginitis is determined by the nature of the infection and the responsible pathogen. Distinct forms of vulvovaginitis necessitate tailored treatment strategies, such as utilizing antifungal remedies for yeast infections, employing antibiotics for bacterial vaginosis, or following particular protocols designed for sexually transmitted infections. The choice of treatment hinges on an accurate diagnosis.
Being informed about suitable vaginal treatments helps in efficiently tackling and controlling vulvovaginitis.
Antifungal Treatments
Oral fluconazole is a highly effective antifungal treatment essential for combatting yeast infections. An individual 150 mg dose of this medication can treat such infections successfully by tackling the excessive growth of Candida albicans and providing relief from symptoms. When dealing with localized yeast infections, patients are often advised to use over-the-counter topical treatments, including clotrimazole and miconazole.
To prevent the recurrence of vaginal candidiasis, maintenance therapy involving weekly doses of fluconazole may be prescribed. Local application of topical antifungal agents like clotrimazole offers an accessible and successful method for treating specific areas affected by infection. Such therapies play a crucial role in both managing current cases and avoiding subsequent occurrences of recurrent vulvovaginal candidiasis.
Antibiotic Treatments
The primary approach to treating bacterial vaginosis involves the use of antibiotics, with oral metronidazole often being the drug of choice due to its higher success rates when compared to topical therapies. Metronidazole can be administered as either an oral treatment or through a combined method using both oral and vaginal treatments, offering versatility in addressing this condition by helping reestablish the vagina’s normal population of healthy bacteria.
An alternative antibiotic known as clindamycin is also utilized in combating vulvovaginitis-related bacterial infections and comes in various forms such as a cream or an orally ingested medication. These therapeutic options are effective for controlling bacterial vaginosis, alleviating symptoms, and aiding in preventing it from coming back.
Managing STIs
Treating vulvovaginitis caused by STIs entails utilizing antibiotic protocols specifically designed for the identified infection. As an example, the medication prescribed for Chlamydia is distinct from what’s administered for gonorrhea, hence a precise diagnosis and specific treatment are imperative. Expedited partner therapy can accelerate healing by enabling individuals to supply their sexual partners with treatments directly, thus reducing the likelihood of becoming reinfected and fostering overall wellness.
To effectively manage STIs, it is essential not only to treat those who are infected, but also to ensure that their sexual partners receive proper medical care. This method contributes significantly to disease control and prevention by disrupting the continuity of reinfections while supporting a healthy vaginal environment.
Home Remedies and Lifestyle Changes
Managing and preventing vulvovaginitis can be greatly enhanced with home treatments and changes in one’s lifestyle. Consider these straightforward strategies.
- Cool compresses, These offer momentary ease for the discomfort and itchiness of vaginal irritation.
- Coconut oil, Its hydrating effects are beneficial in reducing dryness and unease within the vaginal region.
- Warm sitz baths – Utilizing baking soda or colloidal oatmeal during these baths can effectively calm irritated skin around the vagina, diminishing inflammation.
Incorporating such remedies supports symptom management while promoting comfort.
To fend off vulvovaginitis, especially among young girls, adhering to proper hygiene is crucial. Steering clear of strong soaps, bubble baths, and douches helps guard against irritation. Meanwhile, teaching young girls correct wiping methods post-toilet is vital for sustaining vaginal health as well as warding off infections. Such simple yet potent steps play an important role in ensuring overall vaginal wellbeing.
Preventing Recurrent Infections
To mitigate the risk of repeated vulvovaginitis, it’s essential to employ a dual approach that includes medical intervention and changes in personal habits. The strategies include:
- Utilizing maintenance fluconazole therapy consistently can help diminish the occurrence of frequent vaginal infections.
- Opting for loose, cotton undergarments is advised to promote dryness and minimize irritation risks.
- Steering clear of chemical irritants such as fragranced soaps and douches can support maintaining a healthy balance in the vaginal flora.
Incorporating probiotics found in yogurt into one’s diet aids in restoring beneficial bacteria within the vagina, thereby helping counter yeast infections. Effective diabetes management and keeping blood sugar levels under control are also crucial steps toward reducing susceptibility to fungal infections. By adopting these preventative practices diligently, individuals significantly lessen their chances of recurrent infections while fostering optimal vaginal health overall.
Special Considerations for Different Populations
When addressing vulvovaginitis, it’s crucial to consider the distinct needs of various groups such as pregnant women, postmenopausal women, and prepubescent girls. Each demographic experiences unique issues that need specific attention for successful treatment and management of the condition.
Understanding these unique challenges is vital in delivering customized care that will lead to optimal results for individuals suffering from vulvovaginitis within these particular populations.
Pregnant Women
Expecting mothers with vulvovaginitis must exercise caution when treating their condition to safeguard the well-being of their unborn child. The hormonal shifts that occur during pregnancy may disrupt the balance in the vaginal area, rendering pregnant women more prone to infections such as vulvovaginitis. To reduce potential harm to the fetus, treatment strategies typically favor non-systemic methods, and topical imidazole is often recommended for managing vulvovaginal candidiasis.
Ensuring the health of both mother and baby takes precedence while addressing vulvovaginitis amidst pregnancy. Proper management of this condition is crucial in averting negative outcomes associated with pregnancy, including premature labor and infants born underweight. It’s vital for pregnant women to be informed about safe therapeutic approaches at their disposal.
Postmenopausal Women
Women who have gone through menopause are more likely to experience vulvovaginitis due to a decline in estrogen levels, leading to alterations in the vaginal environment. These hormonal shifts typically manifest as increased dryness of the vagina and heightened vulnerability to infections like genitourinary syndrome of menopause, alongside atrophic vaginitis. To relieve these symptoms and promote vaginal health, hormone therapy involving estrogen may be recommended.
As a consequence of reduced estrogen production, many postmenopausal women suffer from atrophic vaginitis which can contribute to Vulvovaginitis issues such as vaginal atrophy. It is essential for managing patient well-being that one understands both why these conditions occur after menopause and what treatments are available for alleviating the associated discomforts so as improve their overall quality of life.
Prepubescent Girls
In prepubescent girls, vulvovaginitis is a common condition often resulting from exposure to irritants and inadequate hygiene. Due to their still-developing immune systems, these young individuals are at an increased risk for both infections and irritation-related discomfort. Effective management of vaginitis involves implementing gentle care practices and providing appropriate instructions on maintaining proper hygiene in order to minimize Aggravation and ward off additional infections.
Key elements in the treatment approach for vulvovaginitis among younger females include regular bathing routines while steering clear of factors that can cause irritant contact dermatitis. In some instances where inflammation or bacterial proliferation is present, clinicians may turn to treatments such as low-dose topical antibiotics or steroids. By prioritizing soft hygiene measures, comfort levels are preserved, contributing significantly toward averting recurrent infections in this susceptible age group.
Sexual Health and Communication
It is imperative to maintain open and honest communication regarding sexual health in order to effectively manage vulvovaginitis, especially when it stems from sexually transmitted infections. By keeping sexual partners informed and ensuring they receive treatment, one can prevent subsequent reinfections and enhance overall health for all individuals involved. Engaging in conversations about STI status not only helps with emotional support but also bolsters commitment to following through with prescribed treatments.
Adhering to safe sexual practices such as consistently using condoms greatly diminishes the likelihood of acquiring STIs that could lead to vulvovaginitis. Implementing strategies that alert partners is crucial in identifying those with undiagnosed STIs, thereby halting the spread of infection and supporting vaginal health.
Placing a strong emphasis on both sexual well-being and communicative transparency is key in averting and addressing vulvovaginitis efficiently.
Summary
Grasping the intricacies of vulvovaginitis is essential for its successful management and therapy. Identifying frequent triggers, including bacterial vaginosis, yeast infections, and sexually transmitted infections (STIs), coupled with implementing correct treatment approaches, can greatly enhance vaginal health. Preventative actions like adhering to proper hygiene practices, steering clear of irritants, and engaging in protected sexual activities are crucial in diminishing the likelihood of recurrent infections. By fostering transparent dialogue and customizing care across various demographics, it becomes possible to secure improved health outcomes and elevate the well-being for individuals experiencing vulvovaginitis.
Frequently Asked Questions
What are the common symptoms of vulvovaginitis?
Common symptoms of vulvovaginitis are abnormal vaginal discharge, itching, burning sensations, and vaginal irritation. The discharge may vary in color and odor based on the underlying cause, such as a fishy smell in bacterial vaginosis or a cottage cheese-like consistency in yeast infections.
How is bacterial vaginosis different from a yeast infection?
Bacterial vaginosis is characterized by an imbalance of vaginal bacteria, leading to a grayish-white discharge with a fishy odor, whereas a yeast infection results from an overgrowth of Candida fungi, causing intense itching and thick white discharge.
Understanding these differences is crucial for proper diagnosis and treatment.
Can vulvovaginitis be prevented?
Vulvovaginitis can be effectively prevented by maintaining proper hygiene, avoiding irritants like harsh soaps, wearing breathable cotton underwear, and practicing safe sex to minimize the risk of STIs.
These preventive measures are essential for maintaining vaginal health.
What are the treatment options for vulvovaginitis during pregnancy?
The treatment options for vulvovaginitis during pregnancy primarily include topical imidazole for vulvovaginal candidiasis, as it minimizes risks to the fetus.
Oral antifungals are typically avoided to ensure the safety of both mother and child.
Why is it important to treat both partners for STIs?
It is essential to treat both partners for STIs to prevent reinfection and effectively control the disease. This approach helps to identify and treat any undiagnosed infections, thereby disrupting transmission chains and promoting overall health.